People who received blood for transfusions before this date might possibly have been exposed to hepatitis C. Hemovigilance programmes which are presently being installed will provide more data on the safety of blood transfusion.
 Hepatitis C Virus Current Studies In Hematology And Blood Transfusion No 62 Reesink H W 9783805565424 Amazon Com Books
Hepatitis C Virus Current Studies In Hematology And Blood Transfusion No 62 Reesink H W 9783805565424 Amazon Com Books
Hepatitis C can also be transmitted through the use of unsterilized medical equipment.
Hepatitis c blood transfusion. The global epidemic of HCV infection emerged in the second half of the 20th century and several lines of evidence indicate that it was primarily triggered and fed iatrogenically by the increasing use of parenteral therapies and blood transfusion. Transfusion-associated hepatitismost of which in retrospect was caused by hepatitis Coccurred in 30 of transfusion recipients prior to the 1970s. Blood transfusions and the sharing of used needles and syringes have been the.
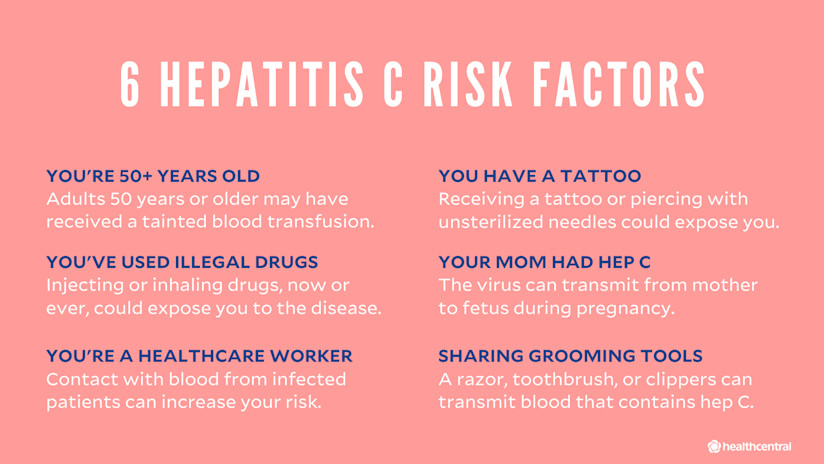
INTRODUCTION In 2000 primary care physicians surgeons and other medical specialists began receiving notification from hospital blood banks that a patient they had previously treated or were currently treating may have been exposed to hepatitis C virus HCV as a result of blood transfusion. All donated blood is thoroughly tested for HIV. Prior to 1992 receiving a blood transfusion or organ transplant was a significant risk factor for contracting HCV.
Cagle HH1 Jacob J Homan CE Williams JL Christensen CJ McMahon BJ. What is the risk of acquiring hepatitis C from transfused blood or blood products in the United States. If you have had an accident or operation in the UK which required a transfusion of blood or blood products before 1991 you may have been exposed to infected blood.
From 30 in 1970 to virtually zero in 2000. Now that more advanced screening tests for hepatitis C are used in blood banks the risk of transmission to recipients of blood or blood products is considered extremely rare at. It has also been linked with malignant lymphomas and autoimmune disease.
The residual risk of HCV transmission due to donations in the anti-HCV window period at present is about 1 in 100 000 transfusions of cellular products and transmission of HCV by plasma products treated with modern inactivation methods such as solvent-detergent treatment has not been reported. Sometimes it is a co-infection with B and C although it does not change the disease process. Results of a general hepatitis C lookback program for persons who received blood transfusions in a neonatal intensive care unit between January 1975 and July 1992.
Hepatitis C Virus HCV is spread primarily by contact with blood and blood products. Hepatitis C is a blood-borne virus meaning that a person must come into contact with blood that contains the virus to contract it. Angelo Magrini the head of a hemophiliacs association said that as of 2001 1300 people including almost 150 children had died in Italy from infected blood infusions since 1985.
However tens of thousands of people got hepatitis c through blood transfusions prior to 1992 and so anyone who had a transfusion before 1992 should be tested for hepatitis c. Hepatitis G HGV or GB virus C GBV-C infection is for the most part with out symptoms. Hepatitis B and C.
It declined to 10 in the early 1970s with the switch from commercial to volunteer blood donors to under 5 when surrogate markers were introduced to screen blood and to almost never 1 in 23 million transfusions with sensitive nucleic acid. The odds of catching hepatitis B from donated blood is about 1 in 300000. Hepatitis C is a serious viral infection that can lead to chronic liver disease liver cancer hepatoma and chronic fatigue syndrome.
For the discovery of the virus that causes hepatitis C and the development of screening methods that reduced the risk of blood transfusion-associated hepatitis in the US. Most new cases of hepatitis C. Hepatitis C infection through blood transfusions or transfusion of blood products no longer occurs because of thorough screening of the blood supply in Canada.
The risk with hepatitis C is 1 in 15 million. In developed countries the rapid improvement of healthcare conditions and the introduction of anti-HCV. It is worth noting that you may not be aware that you were given blood.
Hepatitis C can be passed through sharing personal care items such as toothbrushes nail clippers and razors and condomless sex but no risk is. Our blood supply in the us has multiple mechanisms to reduce the risk of acquiring hepatitis c through transfusion to less than 1 in 16 million. There is a 1 in 2 million chance that donated blood will not only carry HIV but also infect a transfusion recipient.
The infection is very easily spread by transfusion. However this route of transmission is now considered very rare. The Lindsay Tribunal was set up in Ireland in 1999 to investigate the infection of hemophiliacs with HIV and Hepatitis C from contaminated blood products supplied by the Blood Transfusion Service Board.
Thirty years ago the blood transfusion intended to save your life might have killed you. HGVGBV-C is primarily transmitted through blood transfusion. Since September 1991 all blood in the UK has been screened for hepatitis C.
Hepatitis C virus HCV is a leading cause of chronic blood-borne infection and chronic liver disease.
